10 Best Practices for Managing Inventory of Medical Supplies
Managing medical supply inventory is far more than a back-office task; it’s a critical front-line function that impacts patient safety, regulatory compliance, and operational performance. From ensuring personal protective equipment (PPE) is available when needed to keeping surgical tools stocked and sterile, even a single lapse can lead to serious consequences, including treatment delays or compromised care. Financially, mismanaged medical inventory costs the industry billions each year.
What makes managing medical supplies so hard is the number of industry regulations, the variety of storage and usage environments, and the sensitive nature of the products themselves. Many items expire quickly, require cold storage, or must be traceable by lot or batch for safety and compliance. Since COVID-19, unpredictable demand spikes and supply chain disruptions have only added to the urgency of better inventory control.
That’s why implementing proven best practices is essential. These methods help healthcare providers and service-based organizations reduce stockouts, prevent expiration-related waste, automate replenishment, and stay compliant with FDA and audit requirements. In this article, we unpack 10 key strategies to strengthen your approach and skyrocket inventory accuracy across every touchpoint.
10 Best Practices for Managing Medical Supply Inventory
When it comes to medical supplies, there’s no room for error. Whether you're overseeing a hospital, EMS fleet, or outpatient care facility, these 10 best practices will help you prevent stockouts, minimize waste, and improve overall efficiency.
1. Implement Real-Time Inventory Tracking
Real-time visibility into what’s in stock—and where—is foundational to supply availability and cost control. Traditional spreadsheets or manual counts can’t keep up with the pace and complexity of medical supply consumption.
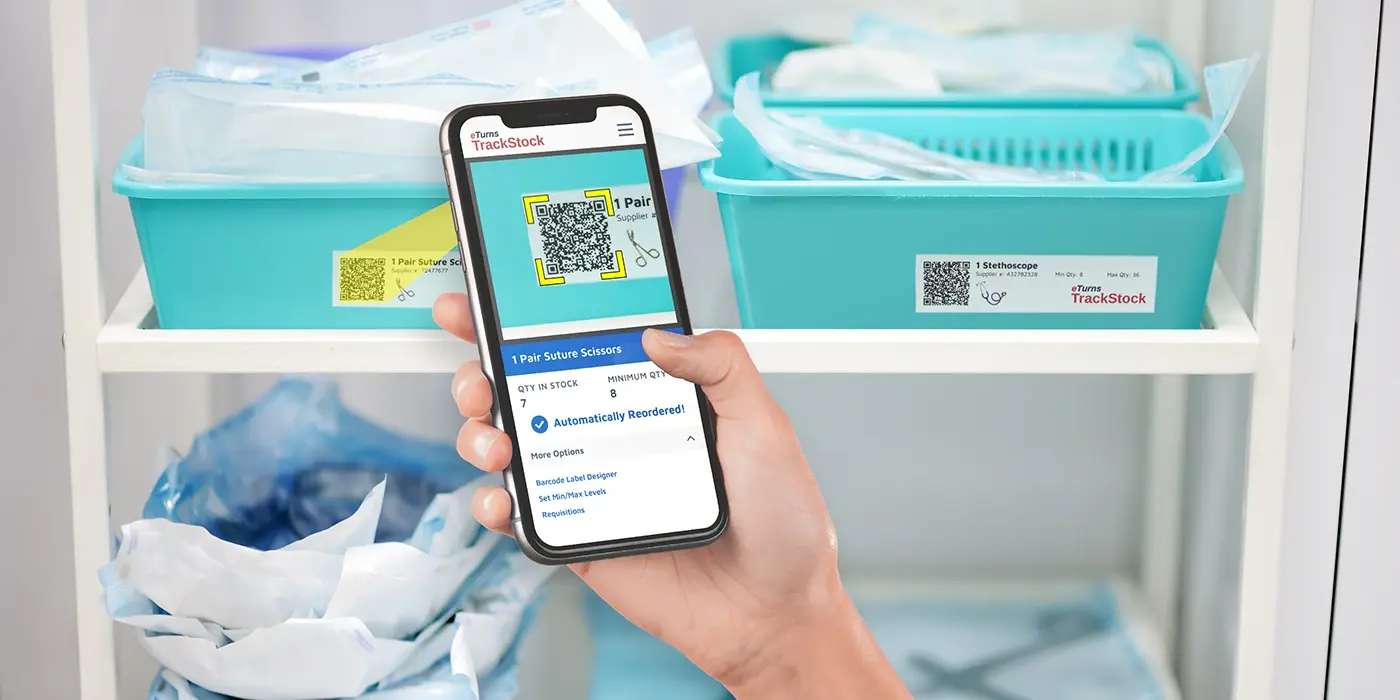
Pro Tip: Use cloud-based inventory software that updates automatically as supplies are issued, scanned, or replenished. eTurns TrackStock, for example, enables tracking across clinics, trucks, and departments, ensuring decision-makers always know what’s available and what’s running low.
2. Use Barcode Scanning or RFID for Accuracy
Manual data entry introduces errors. By contrast, barcode scanning and radio frequency identification (RFID) tagging allow staff to update inventory records with a single scan, ensuring accuracy while saving time.
3. Set Min/Max Levels Based on Usage
Setting reorder points (min) and optimal stock levels (max)–abbreviated as min/max–based on historical usage helps you automate replenishment and avoid both shortages and excess inventory.
Best Practice: Use inventory management software with AI-based min/max tuning capabilities. eTurns’ Min/Max Dashboard recommends and dynamically adjusts levels based on consumption data, lead times, and seasonality.
4. Track Expiration Dates Automatically
Expired supplies can’t be used and pose compliance and safety risks. You need a system that flags products nearing expiration so they can be used or replaced in time.
Quick Tip: Implement a system that allows you to tag items with expiration dates during receiving and provides alerts as those dates approach.
5. Perform Cycle Counts Instead of Annual Counts
Annual physical inventories are disruptive and prone to errors. Cycle counting—a process of checking smaller sections of inventory on a regular basis—is more efficient and accurate.
Why it Works: Regular cycle counts reduce shrinkage, improve inventory accuracy, and help teams stay audit-ready year-round.
6. Automate Replenishment Workflows
Manual reorder processes slow down procurement and increase the chance of stockouts. Auto-replenishment from real-time data ensures supplies are reordered before they run out.
Use Case: An emergency medical services (EMS) provider uses eTurns TrackStock to automatically send purchase orders when supplies like gloves or syringes hit their reorder point. This eliminated their need for paper logs and guesswork.
7. Segment Inventory by Criticality
Not all supplies are equal. Divide inventory into tiers based on importance—life-critical, essential, and non-essential—and manage accordingly.
Strategy Tip: Assign tighter control (e.g., more frequent counts, tighter min/max levels) to critical items like surgical kits or defibrillator pads.
8. Centralize Data Across All Locations
For brands with multiple sites, like urgent care centers and mobile health units, a centralized inventory system provides visibility and control.
Tech Tip: Choose inventory software that supports multi-location tracking with centralized dashboards. This lets you shift inventory of medical supplies between locations when needed instead of placing costly rush orders.
9. Standardize Receiving and Issuing Procedures
Inconsistent processes lead to inaccurate data. By standardizing how supplies are received, labeled, and issued, you improve accountability and reduce errors.
Best Practice: Use mobile apps to scan supplies as they arrive or are dispensed. Track who used what, when, and where, for better traceability and reporting.
10. Monitor KPIs and Audit Performance Regularly
You can’t improve what you don’t measure. Monitor key performance indicators (KPIs) like inventory turnover, order cycle time, and stockout frequency to spot inefficiencies and trends.
KPI Checklist:
-
Inventory accuracy rate
-
Stockout incidents per month
-
Order fulfillment time
-
Expired item write-offs
-
Cycle count variance
Bonus Tip: Set quarterly performance reviews using the analytics dashboards available in your inventory system.
How to Choose the Right Inventory Management System for Medical Supplies
Selecting the right inventory system isn’t just about ticking feature boxes. It’s about finding a solution tailored to your operations, regulatory environment, and supply chain complexity. Here’s a practical step-by-step guide to help you make the right choice for managing your medical supply inventory:
1. Identify Your Primary Inventory Challenges
Start with a quick audit:
-
Are stock outs delaying procedures?
-
Is overstock tying up capital?
-
Are manual processes slowing your team down?
Here are four common issues to look for:
-
Frequent emergency orders.
-
Discrepancies between what’s on the shelf vs. what’s recorded.
-
Time-consuming manual counts.
-
Poor visibility across departments or remote locations.
Understanding your pain points gives you a clear roadmap for evaluating software features.
2. Prioritize Compliance and Traceability
Medical supply inventory must meet high regulatory standards. Choose a system that supports:
-
Expiration date tracking
-
Lot and batch number traceability
-
Audit trail documentation
-
Alerts for recalled or expired items
Pro tip: For healthcare providers, compliance with FDA, HIPAA, or Joint Commission standards is non-negotiable. Look for software vendors who understand these requirements.
3. Look for Features That Support Automation
Automated inventory management saves time, increases accuracy, and reduces waste. Prioritize systems that offer:
-
AI-powered min/max inventory levels
-
Barcode or RFID scanning
-
Auto-replenishment workflows
-
Real-time updates across locations
Automation is especially valuable for EMS, surgical centers, and fast-paced outpatient facilities where supplies move quickly and teams can’t stop to count bins.
4. Consider Integration with Existing Systems
Your inventory software should never be or cause a silo. Make sure it can integrate with:
-
ERP and accounting platforms (like QuickBooks, NetSuite, or Sage)
-
Procurement systems
-
Supplier EDI/API connections
This ensures data consistency, faster order processing, and a clearer financial picture across departments.
5. Assess Mobile Access and Ease of Use
Healthcare teams often need to update inventory on the go. Look for software with:
-
A user-friendly mobile scanning app
-
Zero-touch scanning via SensorBins
-
Cloud-based access for off-site visibility
Example: eTurns TrackStock enables cycle counting, issuing, and auto-replenishment with min/max settings – all done with easy QR code scans—ideal for EMS teams and multi-site clinics.
6. Evaluate Support and Onboarding Services
Even the best system won’t deliver ROI if your team can’t use it effectively. Choose a provider that offers:
-
Guided onboarding and training
-
Responsive customer support
-
Ongoing education (videos, help docs, webinars)
Ask vendors how long it typically takes for customers to go live—and how they support adoption.
7. Request a Trial or Pilot Program
Finally, test before you commit. Most modern inventory systems offer a 14- to 30-day free trial.
Ask yourself the following questions during evaluation:
-
How long does setup take?
-
How intuitive is the interface?
-
Are team members able to adopt it easily?
-
What reporting insights does it provide after a week or two?
A short pilot gives you real-world proof of value—and a better sense of long-term ROI.
Achieving Effortless Efficiency
Managing medical supply inventory isn’t just about keeping shelves stocked—it’s about ensuring patient safety, improving operational efficiency, and controlling costs. In an environment where a single stockout can impact patient care and a single over-order can lead to waste and compliance risk, visibility and precision are everything.
The best inventory strategies combine smart systems, automation, and real-time data. Whether you’re overseeing inventory across emergency vehicles, satellite clinics, or hospital stockrooms, adopting the best practices we covered in this article reduces your shrinkage, eliminates manual work, and keeps your team focused on what really matters: getting results.
If you’re looking for a trusted, proven solution, eTurns TrackStock is purpose-built for healthcare and service teams. Begin your free trial of eTurns now and see how easy it is to manage your medical supply inventory with fewer headaches and more control.




